Program: Food banks and pantries
Takeaways
-
In the United States, food insecurity — or the lack of consistent access to enough food for an active, healthy life — is an important and often hidden problem. In 2015, 15.8 million US households (12.7 percent of the U.S. population) were food insecure at some time during the year.
-
Food insecurity and poor access to healthy foods limit people’s ability to have a balanced diet and places children and adults at higher risk of obesity, diabetes and other diet-related health conditions, anxiety and depression, and reduced academic achievement.
-
Food banks play a central role in the network of national, regional, and local organizations working together to address the needs of food insecure communities across the nation.
-
Because food insecurity and health are interrelated, health care providers have begun to screen patients for food insecurity and connect food insecure individuals to food resources, including food pantries.
-
Hospitals can support food banks and pantries in their efforts to provide fresh, healthy food for their clients
-
Health care facilities can help establish nutrition standards, which is an effective strategy to improve the nutritional quality of the food distributed.
-
Community benefit grants for refrigerators can help food pantries store and distribute fresh food.
-
Hospitals can support programs in which healthy food is sourced from farm gleaning, farmers market gleaning, plant-a-row programs in the local community, as well as from retail sources.
-
Hospitals can also help food banks partner with local farmers to increase the supply of fresh, healthy, local food for families in need and also support local farmers.
-
-
From hosting food pantries onsite to offering diet and nutrition education to investing in mobile pantries there are myriads of ways to leverage the unique and critical partnership between food banks and hospitals.
This brief details opportunities to provide hospital community benefit support to food banks and pantries in order to improve community members’ access to healthy food.
In the United States, food insecurity — or the lack of consistent access to enough food for an active, healthy life — is an important and often hidden problem. In 2015, 15.8 million US households (12.7 percent of the U.S. population) were food insecure at some time during the year.
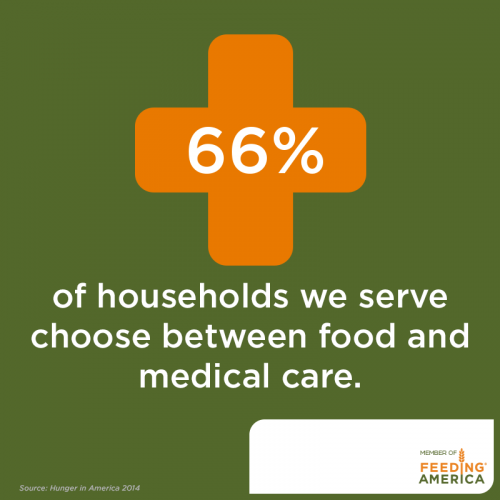
People experiencing food insecurity have poorer quality diets, are more likely to be overweight or obese, and are at greater risk of diet-related chronic health conditions than the general population. Food insecurity may put people in the position of making trade-offs between healthy food, medicine, and other essential needs and makes it more difficult to manage chronic health conditions.
A study of Feeding America food bank clients found that 66 percent of households choose between paying for food and medicine or medical care each year, while 55 percent choose between paying for food and housing.
Food banks play a central role in the network of national, regional, and local organizations working together to address the needs of food insecure communities across the nation.
Food banks secure food donations from the food and grocery industries, government agencies, individuals, and other organizations and make this food available to local charitable feeding programs. Operating like warehouse and distribution centers, food banks receive, sort, review for quality, store, and distribute food to smaller agencies that provide food directly to clients.
Where food banks source and channel food resources at large scale, food pantries provide food directly to food insecure individuals and families in their communities. For example, the Greater Pittsburgh Community (GPC) Food Bank distributes food to over 400 agencies in an eleven-county service area in southwestern Pennsylvania. These agencies are nonprofit community or government agencies, including food pantries, soup kitchens, and homeless shelters. This network of agencies allows the GPC food bank to distribute 26.5 million pounds of food to 360,000 people annually.
Over 200 regional food banks nationwide are members of Feeding America, the largest hunger-relief organization in the United States. Feeding America delivered four billion meals to individuals and families facing hunger in 2016 through various initiatives including food rescue efforts, food pantries, backpack programs, and Supplemental Nutrition Assistance Program (SNAP) Outreach.
Because food insecurity and health are interrelated, many health care providers have begun to screen patients for food insecurity and connect food insecure individuals to food resources including food pantries.
Hospitals can also partner with food banks and pantries to conduct chronic disease screening — a valuable contribution to community health since so many individuals relying on emergency food are living with diet-sensitive chronic disease. In fact, 58 percent of households that rely on the emergency food bank network reported in 2014 that at least one household member has hypertension and 33 percent reported that at least one member has diabetes. Food banks and pantries offer hospitals important opportunities for health interventions to prevent and treat diet-related health conditions.
Challenges for food banks in providing healthier foods
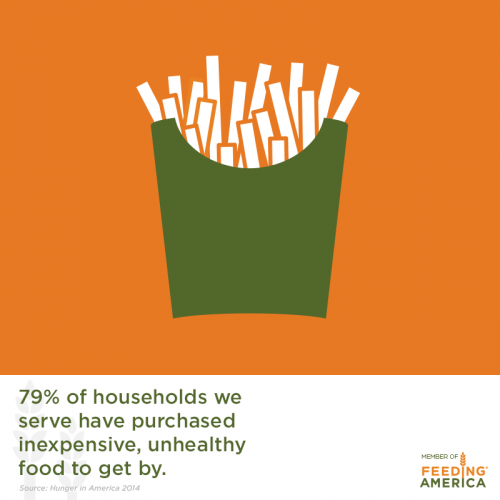
While food banks and food pantries are critical food sources to address food insecurity, they are not always sources of fresh, healthy food. Food banks often receive donations of less-healthy options, including canned or packaged food products that have a longer shelf life and are easy to store and distribute.
In order to address both food insecurity and support healthy diets to prevent and treat chronic disease, food pantries need to provide a variety of healthy foods. However, lack of staff and physical infrastructure and chronic funding shortages can make it difficult for a food pantry to secure and distribute healthy items, especially fresh fruits and vegetables. Many food pantries only distribute food to clients a few times per month or don't have the refrigeration capacity necessary to handle fresh produce. Food pantries can move toward becoming sources of fresh, healthy food. Hospitals can play an important role in supporting these efforts.
Establishing nutrition standards can be an effective strategy to improve the nutritional quality of the food distributed. These standards generally focus on increasing healthy food offerings and eliminating certain unhealthy products by developing criteria to determine what products food banks purchase and what types of donations they will and will not accept. A national survey of 137 food banks found that only 39 percent reported having some type of organizational nutrition policy or guidelines and fewer than a third reported having guidelines to decrease foods or beverages with limited nutritional value (e.g. sugar-sweetened beverages and packaged snacks).
Food banks and pantries may be cautious when implementing strong nutrition standards out of concern that it may reduce the total amount of food available for distribution. Yet this worry may be misplaced. The Capital Area Food Bank (CAFB) received overwhelming support from retail donors when it established its nutrition policies. For example, Giant Food, a key donor, implemented a “Retailers for Wellness” program that sorts out soda, bakery items, and candy from food bank donation bins and prepares nutritious boxes for customers to purchase for donation at checkout.

Farm to food banks
Food banks can partner with local farmers to increase the supply of fresh, healthy, local food for families in need and also support local farmers.
-
Increases the quantity and variety of fresh produce offerings for families seeking support from their local food pantry
-
Helps farmers recover losses. Food banks pay below-market prices for produce that would otherwise not be sold due to cosmetic imperfections or overproduction
-
Reduces food waste that could be better utilized to feed the 41 million Americans that experience hunger daily. Additionally, food waste often ends up in landfills and contributes to greenhouse gas emissions.
The Ohio Association of Food Banks and Kentucky Association of Food Banks (KAFB) are two of the many state food bank associations that have established or are developing farm-to-food bank programs:
-
In 2016, the Ohio Food Program and Agricultural Clearance Program distributed 52.7 million pounds of nutritious food to food banks.
-
In 2017 KAFB Farm to Food Banks program distributed 3,610, 000 pounds of produce to food banks and, as a result, provided 390 farmers with an average of $1,700.
Farm-to-food banks programs offer community benefit departments a great opportunity to increase healthy food access and support food producers in their own communities.

An HonorHealth care coordinator delivers a diabetes wellness box to a patient. Desert Mission Food Bank in Arizona developed a diabetes wellness program to foster healthy food access for patients with diet-related diseases. (HonorHealth)
Recommendations for hospital participation
There are many examples of successful partnerships between hospitals and food banks or food pantries to increase access to healthy foods. These include partnerships that help to expand the reach and improve the quality of foods provided by local food banks and food pantries, providing funding for targeted projects, and helping food banks develop nutrition policies.
-
Healthy food can be sourced from farm gleaning, farmers market gleaning, plant-a-row programs in the local community, as well as from retail sources. Hospital staff can act as liaisons for these initiatives.
-
Hospital grounds can be utilized as gardens to produce donated foods.
-
Hospitals can offer grant support to purchase refrigerators, which are required to sustain the offering of healthy, but perishable goods.
-
Hospital food purchasers may also be able to support food bank staff with identifying vendors for healthy food products or with negotiating pricing.
Additionally, food bank-health care partnerships often include an educational component in which participants learn about nutrition and healthy eating, healthy meal preparation, and also are given a selection of fresh, healthy foods for cooking at home.
Hospital staff members are in a unique position to identify both food insecurity and health risks in patients that would qualify for additional food assistance. Hospitals can assist in the identification and referral of patients and other community members to external food banks, offer in-house emergency food assistance, and offer grant support for mobile food banks and pantries to operate in target communities.
Additional information about hospital community benefit roles and examples are included in the table below.
Examples of hospital roles and participation
Columbia St. Mary’s Hospital, Wis. (Conduct health screenings or food insecurity screenings)
Columbia St. Mary’s Hospital
Milwaukee, Wis.
Columbia St. Mary’s (CSM) operates a community-based clinic providing health screenings, including blood pressure, blood sugar, body mass index (BMI), cholesterol, and diabetes, at Ebenezer Church Diabetic Friendly Food Pantry.
800 families utilized the Ebenezer Food Pantry in 2016. The goal is to increase utilization by 50 families per year for the next 3 years.
15% of healthy food types, as defined by dietitians, were offered in 2016. Goals are to increase healthy food types offered by 5% each year for the next 3 years.
Maury Regional Medical Center, Tenn. (Conduct health screenings or food insecurity screenings)
Maury Regional Medical Center
Columbia, Tenn.
Staff members and physicians identify low-income patients who screen positive for food insecurity in the Emergency Department (ED) and refer them to the on-site healthy food pantry.
The Food Pantry serves approximately 28 patients each month and as of February 2017 served a total of 1,002 patients since opening in 2012.
St. Anthony North Health Campus, Colo. (Fund or lead food and nutrition classes)
![]() St. Anthony North Health Campus
St. Anthony North Health Campus
Westminster, Colo.
St. Anthony staff partners with local food banks to educate clients on healthy foods and nutritional cooking utilizing the USDA “Choose My Plate” as a model.
St. Anthony’s healthy weight education and chronic disease management activities, which included their work with food bank clients, reached 12,461 people in 2016.
Dominican Hospital, Calif. (Fund or lead food and nutrition classes)
![]()
![]() Dominican Hospital
Dominican Hospital
Live Oak, Calif.
Passion for Produce Program
Dominican hospital offers a community benefit grant to a local food pantry to implement a nutrition education and fresh fruit and vegetable distribution program.
Participant interviews revealed improved knowledge and skills for incorporating healthy foods into daily life and adoption of healthier eating behaviors over a 6-month program period.
In 2017 Passion for Produce aims to host 34 sites and distribute 1 million pounds of produce to 1,300 families.
Kaiser Permanente, Calif. (Help food banks develop nutrition policies)
![]()
![]() Kaiser Permanente
Kaiser Permanente
California
Kaiser Permanente staff collaborated with community partners to develop the nutrition policy for Alameda County Community Food Bank. Acceptable purchases and donations included fresh fruits and vegetables, whole grains, and low-fat milk. Unacceptable purchases and donations included soda, anything less than 100% juice, and diet products.
In 2014, over half of the 25 million meals distributed consisted of fresh fruits and vegetables.
St. Vincent Randolph, Ind. (Offer financial support to purchase refrigerators)
St. Vincent Randolph
Winchester, Ind.
Randolph Community Food Pantry
St. Vincent Randolph donated funds to purchase refrigerators for the Community Food Pantry to support sourcing and providing clients with fresh produce. In their 2016 CHNA, St. Vincent committed to working with farmers to provide local food banks/pantries with fresh produce and assemble healthy food boxes and recipes for distribution. The Winchester Area Community and Churches Food Pantry is also located on the St. Vincent campus.
In 2015, St. Vincent held a food drive that provided the Winchester Area Community and Churches Food Pantry with 3,128 lbs of donated food.
Providence Hood River Memorial Hospital, Ore. (Offer financial support to purchase refrigerators)
Offer financial support to purchase refrigerators for fresh foods
![]() Providence Hood River Memorial Hospital
Providence Hood River Memorial Hospital
Hood River, Ore.
Working through the Oregon Food Bank network, Providence Hood River and Orchard View Farms split the cost of a ~$1,000 freezer for a site to provide meals to people experiencing hunger.
490,000 lbs. of food, including fresh produce, was delivered to programs in Hood River, Wasco, and Sherman counties in 2015 through the Oregon Food Bank Network.
Hope Medical Clinic, Mich. (Establish a food pantry on hospital campus)
Hope Medical Clinic
Ypsilanti, Mich.
Choice Pantry
Clinic staff operates the on-site pantry and offers fresh produce, dairy, meat, eggs, and non-perishables for patients and local community members.
Choice Pantry distributed 300,000 lbs. of food each year, including 200,000 lbs. of fresh produce.
Westside Health Clinic, Colo. (Establish a food pantry on hospital campus)
Westside Health Clinic
Denver, Colo.
Denver Food Rescue
Denver Health’s Westside Health Clinic serves as a distribution site for excess healthy foods recovered from participating grocery stores and farmers markets. The clinic is located in a food desert and low-income community.
Westside, in collaboration with four other distribution sites distribute 14,736 lbs. of food and surveyed 111 families in 2016.
Boston Medical Center, Mass. (Establish a food pantry on hospital campus)
![]()
![]() Boston Medical Center
Boston Medical Center
Boston, Mass.
Preventative Pantry
Boston Medical Center (BMC) offers the Preventive Food Pantry for patients with special nutritional needs. These patients are written a pantry “prescription” for use twice a month.
In 2011, 80,500 patients and their families were served by the food pantry.
Hallmark Health System, Mass. (Offer financial support for mobile pantry vehicle)
Hallmark Health System
Massachusetts
The North Suburban WIC Mobile Food Market
Hallmark Health System (HHS) funds and operates a mobile food market that is held monthly at the HHS Women, Infants and Children (WIC) Food and Nutrition Services office and offers free meat, fruits, vegetables, whole grain bread, and dairy items in partnership with the Greater Boston Food Bank.
The mobile market visited ~540 families per month, distributed ~190 tons of food, and benefited ~ 68,141 individuals between FY 2014-FY 2015.
Bon Secours Mary Immaculate Hospital, Va. (Hospital garden provides donations to local food banks)
Hospital garden provides fruit and vegetable donations to local food banks
![]()
![]() Bon Secours Mary Immaculate Hospital
Bon Secours Mary Immaculate Hospital
Newport News, Va.
Community Garden
Mary Immaculate Hospital has a community garden on hospital grounds and donates fresh produce to a local food pantry. Staff from multiple different departments “adopt” plots for maintenance and harvesting.
400 lbs. of produce was donated to a local food pantry in 2016.
Carilion Franklin Memorial Hospital, Va. (Hospital garden provides donations to local food banks)
![]() Hospital garden provides fruit and vegetable donations to local food banks
Hospital garden provides fruit and vegetable donations to local food banks
Carilion Franklin Memorial Hospital
Rocky Mount, Va.
Community Giving Gardens
Carilion Franklin Memorial Hospital offers financial and staff support to Community Giving Gardens, located in food deserts in the community, and donates a portion of that produce to local food banks.
17,400 lbs. of produce was donated to local food banks and a soup kitchen from January 1, 2016 to September 30, 2016.
Northwestern Medical Center, Vt. (Commit staff time to connect local farmers and food banks)
![]() Northwestern Medical Center
Northwestern Medical Center
St. Albans, Vt.
Healthy Roots Collaborative
Northwestern Medical Center founded the Healthy Roots Collaborative (HRC), which includes a gleaning program. Volunteers harvest surplus fruits and vegetables from the field and donate the produce to local food pantries.
HRC worked with 10 farms and delivered over 10,000 pounds of produce to 18 area food pantries and meal programs in 2016
Learn more
Feeding America’s discussion of food bank-health care partnerships provides resources and recommendations for health care organizations and hospitals that are forging partnerships with food banks.
Feeding America’s healthy pantry initiative toolkit provides guidance and strategies for increasing healthy food options at food pantries.
Harvard Law School and Feeding America partnered to release a report on food banks as partners in health promotion including sections on collaboration with hospital community benefit departments and healthy food procurement.
Community Food Centres, located in Canada, offers a toolkit for food banks, hospitals, and relevant stakeholders to transform their emergency food assistance programs into preventative medicine initiatives by incorporating and encouraging healthy foods.
The Public Health Institute published a comprehensive resource for improving healthy food and beverage standards in food banks.
Change Lab Solutions’ Banking on Health resource offers guidance for improving nutrition and beverage standards in food banks.
Northwest Harvest’s Resource Guide for Farm-to-Food Bank Strategies offers guidance for increasing the amount of local, fresh foods in food banks.
Northwest Harvest also published a Promoting Healthy Food Guidebook for improving healthy food signage and selection and nutrition education in food banks.
County Health Rankings & Roadmaps offers guidance, resources, and provides examples for improving healthy food initiatives in food banks.
