Food insecurity screening
Takeaways
- In 2015, 15.8 million U.S. households (12.7 percent of the U.S. population) were food insecure at some time during the year
- Food insecurity and poor access to healthy foods limit people’s ability to have a balanced diet and places children and adults at higher risk of obesity, diabetes and other diet-related health conditions, anxiety and depression, and reduced academic achievement
- When health care providers assess patients for food insecurity, they can:
- Help overcome the stigma of food insecurity
- Tailor clinical care to real patient needs
- Identify a vulnerable target population
- Help reduce the prevalence of food insecurity and its effects on the community
- Potentially reduce health care costs by reducing preventable emergency department and provider visits
- Hospitals and health care facilities have incorporated food insecurity screenings into their practice in a number of ways.
- Conducting food insecurity screening in community clinics
- For all patients entering the emergency department
- For youth/adolescent or elderly patients
- As a part of a larger social needs assessment
- Incorporating food insecurity assessment data in electronic medical records
- Many hospitals and health systems throughout the country are incorporating food insecurity screening as part of their standard patient intake procedures. This brief discusses recommendations and screening tools to include food insecurity screening as a part of clinical care.
- Benard P. Dreyer, MD, FAAP, President, American Academy of Pediatrics (2016)

Food insecurity is an important and often hidden problem in the United States. In 2015, 15.8 million U.S. households (12.7 percent of the U.S. population) were food insecure at some time during the year.
Food security is defined by the U.S. Department of Agriculture (USDA) as “access by all people at all times to enough food for an active, healthy lifestyle.” When access to healthy food is hindered by economic barriers, physical limitations, or both, the result is food insecurity.
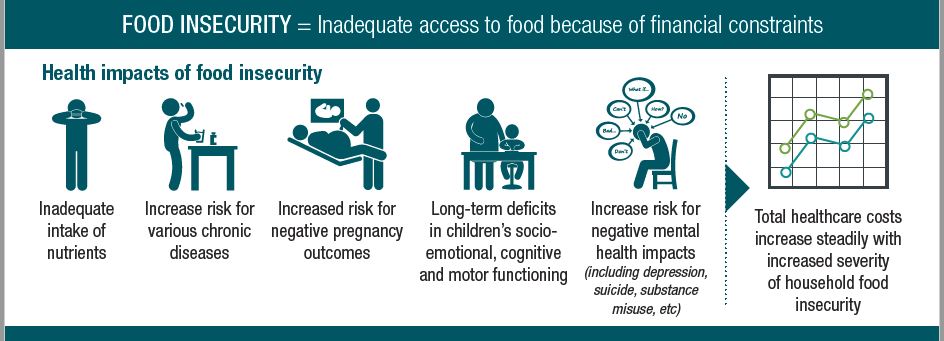
Food insecurity and poor access to healthy foods limit people’s ability to have a balanced diet and places children and adults at higher risk of obesity, diabetes and other diet-related health conditions, anxiety and depression, and reduced academic achievement. Food insecurity may put people in the position of making trade-offs between healthy food, medicine, and other essential needs, and makes it more difficult to manage chronic health conditions. A study of Feeding America food bank clients found that 66 percent of households choose between paying for food and medicine or medical care each year, while 55 percent choose between paying for food and housing.
Why should hospitals conduct food insecurity screenings?
Food insecurity can:
- Mask underlying health conditions
- Cause misdiagnosis
- Prolong hospital stays
- Affect medication adherence
- Contribute to greater use of emergency department and higher health care costs
Health care providers are trusted by their patients as sources of knowledge and guidance to support health and well-being. However, the stigma associated with food insecurity may prevent individuals from mentioning the situation with their providers or seeking assistance. When hospitals and health clinics assess patients for food insecurity, they can:
- Help overcome the stigma of food insecurity
- Tailor clinical care to real patient needs
- Identify a vulnerable target population
- Help reduce the prevalence of food insecurity and its effects on the community
- Potentially reduce health care costs by reducing preventable emergency department and provider visits
Many hospitals and health systems throughout the country are incorporating food insecurity screening as part of their standard patient intake procedures. Food insecurity screenings conducted in the hospital or in the community may be part of determining eligibility for participation and enrollment in community benefit-supported programs. See our guidance brief on reporting community benefit support for healthy food access programs on IRS Form 990 Schedule for guidance on when and how to report community benefit support for food insecurity screenings.
Two-question screening tool
Children’s HealthWatch has developed the Hunger Vital Sign™ two-question screening tool to assess food insecurity in clinical settings. While other food insecurity screening methods are available, this validated tool has become a nationally accepted standard due to its ease of use in clinical settings. This 2-question screener has been endorsed by the American Hospital Association, The American Academy of Pediatrics, and Feeding America, among others. Numerous hospitals and health care systems have integrated the screening tool into their practice including ProMedica and Kaiser Permanente. The questions are written at a 5th-to 6th-grade reading level to facilitate use across a wide range of age groups and literacy levels.
“Within the past 12 months, we worried whether our food would run out before we had money to buy more.”
“Within the past 12 months, the food we bought just didn’t last and we didn’t have money to get more.”
Individuals are asked to respond by answering often true, sometimes true, or never true. If the response to either statement is often true or sometimes true, the individual is identified as food insecure.
Other screening tools
The two-question screening tool was originally derived from the 18-item food security survey developed by the USDA Economic Research Service (ERS) in 1995. This survey module includes adult-referenced questions, youth-referenced questions, and measures the severity of food insecurity. An abbreviated six-item short form food security survey is also available.
The two-question screening tool was also incorporated into the 10-item social screening, which has been developed, validated, and recommended by The Center for Medicaid and Medicare Services. The screening includes five unmet health-related social needs, including access to food and homelessness.

Incorporating food insecurity screening in electronic medical records
It is important that hospitals establish standard methods and infrastructure to screen for food insecurity and other social needs and document those needs in the health record. Supporting a streamlined process will facilitate smoothly incorporating social needs screening into facilities’ standard of care. The incorporation of food insecurity screenings into electronic medical records (EMRs) is important for data collection, analysis, and evaluation efforts, and is also essential for a streamlined referral. Food insecurity screenings can be embedded into EMR systems; for example, the Hunger Vital Sign™ screener is already built into the Epic Foundation System (under “Hunger Screening”). Other biophysical indicators, such as body mass index (BMI) and blood sugar level (hemoglobin A1C) can be tracked in conjunction with food insecurity screenings to evaluate the impact of food and nutrition interventions.
Connecting food insecure individuals to resources
When individuals screen positive, referrals should be made to local organizations that can connect food insecure individuals and families to resources such as the Supplemental Nutrition Assistance Program (SNAP), Special Supplemental Nutrition Program for Women, Infants and Children (WIC), and food pantries. There may be additional resources and initiatives in the community such as fruit and vegetable incentive programs or subsidized community supported agriculture (CSA) shares that can further increase access to healthy food. See further discussion of recommendations and resources for connecting food-insecure individuals and families to food resources.

Flint Fresh Mobile Market, a project initiated through the RFSN program, aggregates produce from local farmers and brings fresh produce to neighborhoods lacking fresh food access each week (Community Foundation of Greater Flint)
Training and implementation
The American Academy of Pediatrics, the Food Research & Action Center, and Feeding America provide training resources and toolkits for effective implementation of food insecurity screenings. While the screening tool itself is standardized and straightforward, the delivery of the screening is essential to reduce the risk of patients feeling shame, embarrassment, anger, or judgment. These emotions will likely reduce patient receptiveness to external support if they qualify for referral. Food bank-health care partnerships have found evidence-based support for written screenings in producing the most honest responses. The following steps can be taken to ensure sensitive delivery: normalization of the screening question, screening in privacy away from other patients, staff, and children, and offering the tool in the patient’s native language.
Recommendations for hospital participation
Hospitals and health care facilities have incorporated food insecurity screenings into their routine practice in a number of ways. Examples include conducting food insecurity screening in community clinics, for all patients entering the emergency department, for youth/adolescent or elderly patients, as a part of a larger social needs assessment, and incorporating food insecurity assessment data in electronic medical records.
Examples of hospital roles and participation
Kaiser Permanente, Colo. (Incorporate food insecurity screening into ER routine intake)
Incorporate food insecurity screening into routine intake of all patients entering emergency department.
![]()
![]() Kaiser Permanente
Kaiser Permanente
Colorado
Kaiser staff in 10 different emergency departments and over 10 medical offices administer the 2-question screener at each patient visit.
Kaiser staff positively screened and referred 1,829 patients since between 2012-2016.
Hennepin County Medical Center, Minn. (Incorporate food insecurity screening into intake for all elderly patients)
Conduct food insecurity screening as part of intake for all elderly patients
Hennepin County Medical Center’s Senior Care Clinics
Augustana and Parkside, Minn.
Staff at HCMC’s senior care clinics conduct food insecurity screenings at every patient visit.
The program resulted in a 1,000% increase in referrals for food insecure patients.
Kaiser Permanente, Ore. (As part of a wider social needs screening)
As part of a wider social needs screening
![]()
![]() Kaiser Permanente Northwest
Kaiser Permanente Northwest
Oregon
Staff employed by Kaiser Permanente Northwest have integrated food insecurity screening questions into their “life situation form” distributed at each patient visit.
One study revealed a 40% decrease in emergency department utilization after Kaiser began their social screening program.
Boston Medical Center, Mass. (As part of a wider social needs screening)
As part of a wider social needs screening
![]()
![]() Boston Medical Center
Boston Medical Center
Boston, Mass.
Staff from Boston Medical Center (BMC) sat on an expert advisory panel to develop the CMS validated 10-item social screening tool, which includes the Hunger Vital Sign™ food insecurity screening tool. This tool has also been implemented into the standard of practice at BMC.
Physicians in BMC’s emergency department and at more than 20 clinics screen patients for food insecurity and write prescriptions to their on-site food pharmacy. These referrals contribute to the pharmacy’s statistic of serving 7,000 people each month.
Massachusetts General Hospital, Mass. (As part of intake in community clinics)
As part of intake in community clinics
![]() Massachusetts General Hospital Primary Care Clinics
Massachusetts General Hospital Primary Care Clinics
Revere and Chelsea, Mass.
Staff at Revere and Chelsea primary care clinics screen all patients for food insecurity.
In 2015 1,830 patients were screened for food insecurity in pediatrics, adult medicine, and prenatal at MGH Chelsea.
Arkansas Children’s Hospital (As part of intake in community clinics)
As part of intake in community clinics
![]() Arkansas Children’s Hospital
Arkansas Children’s Hospital
Little Rock, Ark.
Staff at Arkansas Children’s Hospital implemented a pilot program to screen for social determinants of health at a clinic.
In 2016 7,048 individuals were screened and 2,074 were identified as food insecure.
Memorial City Medical Center, Texas (Conducted for an external organization)
Conducted for an external organization (WIC office, community center, etc.)
Memorial City Medical Center
Houston, Texas
Memorial City provides funding for patient navigators to conduct food insecurity screening in the emergency department, at clinics and might provide some social screening at local food banks in addition to educational services. A services coordinator also conducts a social needs screening at a local, school-based food pantry.
According to a 2017 food insecurity report in Houston and Harris County, Memorial Hermann has positively screened 27% of emergency department patients for food security, 30% in school-based clinics, and 15% in neighborhood clinics.
Promedica Health System, Ohio (Incorporated into EMR system)
Incorporated into EMR system
Promedica Health System
Ohio
Staff at Promedica Health System hospitals and health centers have integrated food insecurity questions into their EMR systems, which facilitates food insecurity screening at each patient visit.
In 2016 57,224 patients were screened for food insecurity.
Greater Lawrence Family Health Center, Mass. (Incorporated into EMR system)
Incorporated into EMR system
Greater Lawrence Family Health Center
Lawrence, Mass.
Staff at GLFHC administer the two-question food insecurity screener at each patient visit and at their on-site farmers market. Results are now a part of each patient's EMR.
Staff screened 1,200 patients for food insecurity
67% of the total patients screened were identified as food insecure.
Learn more
Feeding America offers a training for health care providers conducting food insecurity screenings in a clinical setting. This training includes recommendations for referral after a positive food insecurity screening has occurred.
Feeding America and Humana published a “Food insecurity and health toolkit for physicians and health care organizations” to assist health care professionals in screening for food insecurity and connecting patients to resources.
The Catholic Health Association offers a brief introduction to the social determinants of health and includes links to national initiatives, research reports, tools, models, frameworks, and other resources.
American Academy of Pediatrics and the Food Research & Action Center provides a detailed toolkit for pediatricians incorporating food insecurity screening into their practice.
The University of San Francisco published a comprehensive resource for implementation of food insecurity screenings in a clinical setting that highlights the importance of EMRs and evaluation.
The Nutrition & Obesity Network Policy Research and Evaluation Clinical Linkages Subgroup developed food insecurity tools for the following populations: pediatric patients, adults, and patients living with diabetes.
Health Leads, a national nonprofit organization, has developed a social needs screening toolkit that provides an overview of essential components of screening and its implementation, recommended needs to be included, and sample questions and screening tools for each need.
The Health Research and Educational Trust, an affiliate of the American Hospital Association, recently released a guide discussing food insecurity and the role of hospitals.
California Food Policy Advocates released a report outlining the ways in which health care facilities can use food insecurity screening tools in their practices and increase the number of referrals to food and nutrition assistance programs.
Social Interventions Research & Evaluation Network developed a brief reviewing the evidence and various research projects studying the integration of food insecurity screening in health care settings.
