Program: Fruit and vegetable incentives
Takeaways
- Fruit and vegetable prescription programs partner with health care providers to enroll patients and other community members with nutritional needs in programs featuring “prescriptions” with coupons that can be redeemed for fresh produce.
- Double Up coupons reduce economic barriers to healthier foods by matching the value of Supplemental Nutrition Assistance Program (SNAP) dollars spent on produce. Double Up has served over 1.1 million low-income families and partnered with over 500 farmers markets and 200 grocery stores.
- Across the country, these initiatives are demonstrating promising results:
- A program implemented in New York City increased fresh produce access for 2,755 patients and household members and led to $185,000 in increased sales at local farmers markets.
- Fresh Approach, an organization that coordinates programs in the San Francisco Bay Area, found that 89 percent of participants reported eating more vegetables since the program began.
- Fresh Prescription, a program in Detroit, found a statistically significant decrease in hemoglobin A1c levels for participating low-income diabetics.
- There are several ways that hospitals can provide community benefit support to add value to fruit and vegetable incentive programs.
- Taking a lead role in managing the programs or partnering with another organization or coalition that is managing the program.
- Providing grant support
- Providing staff time and expertise to carry out program components.
- Working with community partners to secure continued, sustainable funding for the program.

Low-income families are more vulnerable to diet-related health conditions, such as diabetes and heart disease, which are exacerbated by limited access to healthy foods. Fruit and vegetable incentive programs such as Double Up Food Bucks and produce “prescriptions” reduce economic barriers that some families face when purchasing fresh, healthy foods by doubling the value of Supplemental Nutrition Assistance Program (SNAP, formerly known as food stamps) resources used to purchase fresh fruits and vegetables or providing vouchers that can be redeemed for fresh produce.
The Fair Food Network, the pioneer of fruit and vegetable incentive programs, initiated the Double Up program at farmers markets in Detroit in 2009. Double Up coupons provide support for healthy food purchasing for individuals and families receiving nutrition benefits from the federal government by matching the value of SNAP dollars spent on produce. Communities in 18 states have adopted the model. Since inception, Double Up has served over 1.1 million low-income families and partnered with over 500 farmers markets and 200 grocery stores.
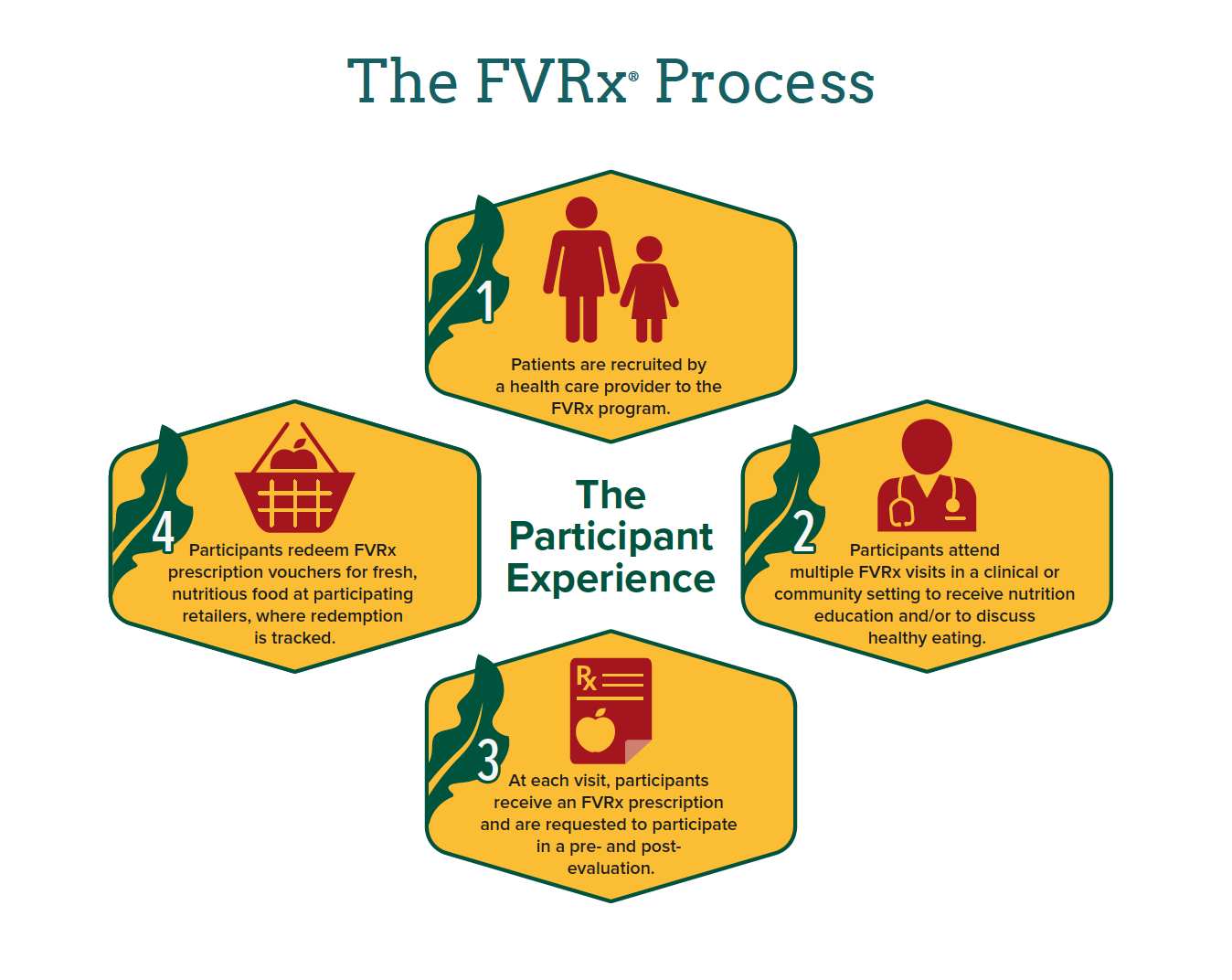
Wholesome Wave, another leader of fruit and vegetable incentive programs, works with community partners to support the growth, quality, and reach of fruit and vegetable prescription (FVRx) initiatives nationally. Fruit and vegetable prescription initiatives partner with health care providers to enroll patients with nutritional needs in programs featuring “prescriptions” with coupons that can be redeemed for fresh produce. Wholesome Wave offers several support systems for members including the sharing of tools and best practices, consulting, and network building.
Wholesome Wave encourages strategies that maximize the multiple potential benefits of FVRx programs including improved patient health, increased produce sales, and local economic growth. Between 2012 and 2015 a Wholesome Wave FVRx program implemented in New York, N.Y. increased fresh produce access for 2,755 patients and household members and led to $185,000 in increased sales at local farmers markets.
Fresh produce incentive programs typically are paired with an educational component in which participants learn about nutrition and healthy eating, healthy and economical shopping, and healthy meal preparation, and also taste new dishes featuring fresh, local produce.
Many health care facilities throughout the country are participating in fruit and vegetable incentive programs as a way to address food insecurity, obesity, and diet-related health conditions in their communities.
Recent evaluation data from fruit and vegetable incentive programs is further building support for these initiatives. 1 2 3
Fresh Approach, an organization that coordinates Veggie Rx programs in the San Francisco Bay Area, found that 89 percent of participants reported eating more vegetables since the program began. Fresh Prescription, a fruit and vegetable incentive program in Detroit, found a statistically significant decrease in hemoglobin A1c levels for participating low-income diabetics. Similarly, Geisinger Health found a decrease in hemoglobin A1c levels for participants in their Fresh Food Pharmacy program. Evaluators of this program found an additional health cost savings of $300 per person, per quarter for participants compared to those who did not participate in the program.
— Bethany Thompson, Veggie Rx client

Local food and vibrant communities
Fruit and vegetable incentive programs are designed to not only increase the affordability of fresh, healthy food for low-income consumers — but also to support local food producers and keep food dollars circulating in the local economy, which can benefit the entire community.
Double Up, Wholesome Wave, and related initiatives are rooted in farmers markets and a commitment to supporting regional and sustainable producers. Produce incentive programs provide new sales and support family farmers, enabling farmers to hire more staff, diversify what they grow, and purchase needed equipment.
While incentive coupons can be utilized in farmers markets, often they can be redeemed in retail outlets. Grocery stores participating in incentive programs expand their product offerings, increase produce sales, attract new SNAP customers, and increase SNAP purchases.
Fruit and vegetable incentive programs have the greatest impact when there are a variety of participating farmers markets (including mobile markets) grocery stores, and corner stores located in areas of greatest need. All participating retailers/vendors need to accept Electronic Benefit Transfer (EBT)/SNAP benefits in order to facilitate use by target populations.
Fruit and vegetable incentive programs can be an effective component of hospital community benefit implementation strategies to address diet-related health needs. Hospital support can increase access to healthy foods, reduce risks for diet-related health conditions, reduce health care costs, and promote community development by supporting local and sustainable producers.
Community partners and program implementation
Diverse contributors and organizations play important roles throughout the process, from identifying eligible program participants (through food insecurity screening or health screenings), enrolling participants in the program, establishing farmers market and retail partners and establishing reimbursement mechanisms, securing sustainable financing of the incentive vouchers, carrying out the educational components, and conducting program evaluation.
Community partnerships are essential for successful incentive program implementation. It is recommended that hospitals partner with organizations that have common goals and capabilities to implement exemplary programs.
Hospital or program staff often work with local food pantries, Women, Infants and Children Food and Nutrition Services (WIC) offices, supplemental or congregate meal sites, community clinics, community food advocacy organizations, or other social service organizations to conduct food security and biometric screenings, enroll participants, provide nutrition education and healthy behavior coaching, and refill “prescriptions” or coupons.
Individuals who screen positive for food insecurity and/or suffer from obesity or a diet-related disease are eligible for enrollment in incentive programs. Fruit and vegetable prescription and Double Up programs typically last 12-16 weeks, a time period that corresponds to the summer growing season as well as to the time needed to adopt health behavior change. However, some incentive programs have different structures, with longer or shorter duration.
Wholesome Wave recommends that incentive amounts follow a $1/day per household member model, and the funding should support this. Following this model, families of four would receive approximately $28-$30 per week. Providing incentive amounts based on the household size can reduce household food insecurity while also promoting behavior change that can be sustained through the participation of the whole family.
The $1/day per person per household standard was determined based on research conducted by Harvard University studying the difference in cost between healthy and “unhealthy” dietary patterns. Because funding the vouchers is the major component of program costs and because programs want to reach as many households as possible, it can be useful to set a cap on voucher amounts. For example, households with more than four members would receive $35 per week regardless of the number of additional members.
Common funding sources for fresh produce incentive programs include federal funding, state funding, and private foundations. Food Insecurity Nutrition Incentive (FINI) Grants are important federal funding sources for projects that provide incentives at the point of purchase for low-income consumers and were developed in response to the significant impact that Double-Up incentives had on fruit and vegetable consumption by SNAP clients. Fair Food Network and the Wholesome Wave websites provide guidance on how to establish incentive programs, including funding mechanisms.
Hospital community benefit grants can be an important source of funding.

Montefiore participates in Health Bucks, a fruit and vegetable voucher program run by New York City. Montefiore has a 98 percent redemption rate for the Health Bucks that they distribute (Montefiore Medical Center)
- Noah Fulmer, Program Director, Fair Food Network
Recommendations for hospital participation
There are several ways that hospitals can provide community benefit support to add value to fruit and vegetable incentive programs.
Hospitals can take a lead role in managing the programs or partner with another organization or coalition that is managing the program. Key roles include providing grant support and providing staff time and expertise to carry out program components. Hospital community benefit staff can also play an important role in working with community partners to secure continued, sustainable funding for the program.
Examples of hospital roles and participation
Mid Columbia Medical Center, Ore. (Conduct health and/or food insecurity screenings to determine eligibility for enrollment)
Mid Columbia Medical Center (MCMC) Clinics
multiple cities, Ore.
Gorge Grown’s Veggie Rx
Participating MCMC clinics screen patients for food insecurity utilizing the validated Hunger Vital Sign™ screening tool. Eligible patients are enrolled in the program and receive incentive coupons.
Almost 800 people were screened for food insecurity and 30% were identified as eligible for the Veggie Rx program in 2016.
Munson Medical Center, Mich. (Distribute prescriptions)
Munson Medical Center
Traverse City, Mich.
Provides patients with chronic disease with fruit and vegetable coupons for use at the local farmers market. 53% of participants also reported that they had skipped meals because there was not enough money for food.
170 patients redeemed $10,650 worth of fruit and vegetable coupons at the local farmers market in 2016.
Adena Health System, Ohio (Distribute prescriptions)
Adena Health System
Chillicothe, Ohio
Fresh Food Rx
Nurse navigators and physicians at Adena give patients with financial need or a chronic illness a $15 Fresh Food Rx coupon.
Evaluation metrics are being collected for the first year of the program (2017).
Seattle Children’s Hospital, Wash. (Provide grant support to fund the incentives)
![]() Seattle Children’s Hospital
Seattle Children’s Hospital
Seattle, Wash.
Fresh Bucks Seattle
Seattle Children’s offers grant support to fund the city’s fresh produce incentive program.
Fresh Bucks participant surveys found an 88% increase in consumption of fruits and vegetables.
Fresh Bucks coupons contributed $330,607 to local farmers and $591,786 to supporting the local economy.
Saint Joseph Mercy Health System, Mich. (Provide grant support to fund the incentives)
![]() Saint Joseph Mercy Health System (SJMHS)
Saint Joseph Mercy Health System (SJMHS)
Southeast Mich.
Prescription for Health
Saint Joseph Mercy Health System provides funding for Washtenaw County Public Health’s Prescription for Health program.
“73% of participants reported that they or others in their home had cut the size of meals, skipped meals, and/or bought fewer healthy foods within the past year because of a lack of money for food.”
Participants reported increasing their fruit and vegetable consumption by over a half a cup a day post-program.
$21,385 worth of prescriptions was spent on fruits and vegetables at local farmers markets.
Providence Hood River Memorial Hospital, Ore. ( Provide staff time/technical assistance to secure funding)
Provide staff time/technical assistance to develop grant proposals to secure additional incentive funding
![]() Providence Hood River Memorial Hospital
Providence Hood River Memorial Hospital
Hood River, Ore.
Veggie Rx
Providence Hood River provided funding for a Community Impact Health Specialist, from 2014-2016, to serve as a grant writer and provide technical assistance for organizations in the area working to meet needs identified in the CHNA, including The Gorge Grown Food Network.
Gorge grown received $20,000 from The Oregon Community Foundation, hospital funding, and financial support from the Tofurky Company for a total of over $30,000 to implement the program in 2015.
Geisinger Health System, Penn. (Operate a produce distribution point for coupon redemptions)
![]() Geisinger Health System
Geisinger Health System
Shamokin, Penn.
Fresh Food Pharmacy
Food insecure, diabetic patients receive prescriptions to utilize at the Fresh Food Pharmacy on the hospital’s campus.
During the implementation of the pilot program in 2016 participant Tom Scowich lost 45 pounds and dropped his A1c level from 11 to the high-6 range.
Harlem Hospital Center, N.Y. (Conduct diet and nutrition education)
Harlem Hospital Center
New York City, N.Y.
Health Bucks
Primary care providers and nutritionists conduct individualized nutritional counseling for participants.
50 low-income families were enrolled in the FVRx program at HHC in 2013.
In 2013, 97% of children and 96% of families reported that they consumed more fruits and vegetables after enrolling in the program at HHC and Lincoln Medical Center.
Harborview Medical Center, Wash. (Conduct diet and nutrition education)
![]()
![]() Harborview Medical Center
Harborview Medical Center
Seattle, Wash.
Fresh Bucks Seattle
Dieticians at Harborview offer group and one-on-one healthy cooking classes for participants in the Fresh Bucks program.
Behavior change surveys found that 89% of participants attributed Fresh Bucks to making a difference in their families diets in 2016.
Florida Hospital Carrollwood (Assist with data collection, data analysis, and evaluation)
Florida Hospital Carrollwood
Tampa, Fla.
Food Is Medicine
Florida Hospital Carrollwood staff administers pre- and post-intervention behavioral checklists and conducts health screenings during the first and last nutrition education classes.
Health screening data revealed that 50% of participants decreased their blood pressure and blood sugar and 25% recorded weight loss in 2015.
Providence Hood River Memorial Hospital, Ore. (Assist with data collection, data analysis, and evaluation)
Providence Hood River conducted a community-based participatory evaluation of Gorge Grown’s Veggie Rx program via their research facility, the Center for Outcomes, Research and Education (CORE).
Increased access to food reduced sense of shame and injustice in participants and allowed them to relax and spend time with their families. “My kids are free to be just kids,” said one participant.
Lankenau Medical Center, Penn. ( Assist with data collection, data analysis, and evaluation)
![]() Lankenau Medical Center
Lankenau Medical Center
Wynnewood, Penn.
Philly Food Bucks
Lankenau incorporates food insecurity screening, referral of food insecure patients to Philly Food Bucks, and participant behavior change into their electronic medical record (EMR) to facilitate evaluation of the impact of this intervention.
432 Philly Food Bucks coupons were distributed from May to November 2014, and health educators conducted 764 health screenings at farmers markets.
Learn more
National support organizations
Wholesome Wave offers membership to their National Nutrition Incentive Network, which facilitates collaboration among relevant stakeholders, provides access to evidence-based tools and resources, and offers online technical assistance and training.
The Fair Food Network provides support for health care organizations implementing fruit and vegetable incentive programs. Resources provide guidance on program design, implementation, and evaluation, including data collection and analysis.
Regional organizations and programs
Fresh Approach, an organization that supports healthy food access initiatives in the San Francisco Bay Area, shares descriptions of its program design, implementation, and evaluation processes. The resource includes discussion of the Veggie Rx diet and nutrition education component.
The Gorge Grown Network (Oregon) Veggie Rx program, which offers both fresh produce vouchers and SNAP matching benefits for eligible participants, provides valuable evaluation tools and other resources.
Other resources
Johns Hopkins Center for a Livable Future’s “Hospitals and Healthy Food” policy brief discusses how hospital community benefit resources can match and extend the reach of Food Insecurity Nutrition Incentive (FINI) grants to support fruit and vegetable incentive programs.
