Empowering health through dignity and trust
Takeaways
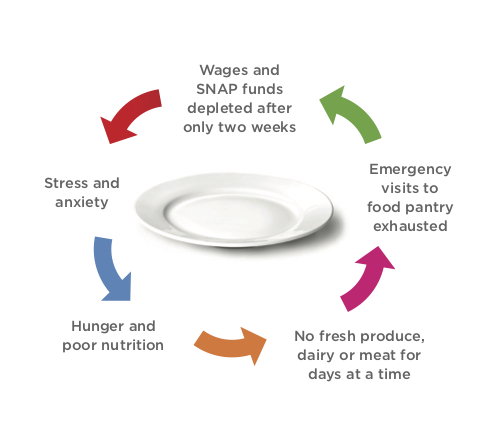
- Kent County faces public health challenges related to rising obesity rates and mental health. Data shows disparities are compounded by issues of poverty, racism, and access to healthy food.
- Obesity has risen by 11 percent since 1993.
- 1 in 6 people is living in poverty.
- 1 in 3 use food assistance programs.
- Over 128 organizations with expertise ranging from food security to housing and seven health care facilities participated in a collaborative community health needs assessment process.
- Spectrum Health has made significant investments of staff time, in-kind resources, and grant funding to programs working to address food insecurity and diet-related disease.
- Partnered with Access of West Michigan to run Nutritional Options for Wellness (NOW), a produce and healthy living prescription program.
- Provides financial and in-kind support to the Community Food Club of Grand Rapids, an innovative membership-based community grocery store.
- The NOW program has been remarkably successful by all available metrics. In 2016, there were 231 participants. Of participants surveyed:
- 97 percent reported that their overall health improved
- 70 percent reported fewer visits to the emergency department
- 90 percent reported that they are cooking healthier for their families and friends.
- The Community Food Club has welcomed 2,086 member households, for a total of 2,505 since opening in 2015.
- Distributed an estimated $801,000 worth of food
- Grew to become the single highest food distribution outlet within Feeding America West Michigan’s 40 county territory
- Sold almost twice as much produce as a traditional grocery store, fruit and vegetables represented 35 percent of grocery items selected.
- After 12 months of membership, 79 percent of respondents stated: "My family and I eat more fruits and vegetables now."
- Spectrum Health was awarded the 2016 Foster G. McGaw Prize through American Hospital Association
- Hospital name: Spectrum Health Butterworth Hospital
- Hospital type: Private, nonprofit
- Hospital size: Large (1102 Beds)
- Geographic area: Metropolitan (Grand Rapids-Wyoming, MI)
- System/network: Spectrum Health System
- Network coverage: West Michigan
- White: 82.4%
- Hispanic: 9.8%
- Black/African American: 9.6%
- Asian: 2.3%
- American Indian: 0.4%
- Community Health Needs Assessment region: Kent County
- Population: 609,544
- Youth obesity: 1 in 4 middle/high-schoolers overweight or obese
- Rising obesity trend: 11% increase since 1993
- Poverty: 1 in 6 living in poverty (15.5%)
- Food assistance: 1 in 3 (32.5%) use food assistance programs
Spectrum Health is a nonprofit, integrated health system in West Michigan that offers a continuum of care through the system’s 12 hospitals, a network of care facilities and physician practices that span 13 counties throughout West Michigan. Spectrum is West Michigan’s largest employer and is headquartered in Kent County in the city of Grand Rapids — Michigan’s second largest city.
Kent County is located on the Western side of Michigan’s lower peninsula, about 30 miles east of Lake Michigan and is comprised of 21 townships, five villages, and nine cities. A significant portion of Kent County’s geographic area is considered rural, however, most of the population resides in urbanized areas or urban clusters.
The vast majority of Kent County residents are white (82.4 percent) and young people (24-54 years old) make up 41.2 percent of the population. Home to several colleges, universities and health care resources, Kent County fares relatively well when it comes to socioeconomic factors such as unemployment, education, and income. However, Kent County has experienced a recent steady increase in population resulting in a lack of affordable housing and growing housing discrimination.
Kent County faces public health challenges related to rising obesity rates and mental health. The county falls short of national benchmarks when it comes to factors such as healthy food and violent crime. A closer look at the data shows evident disparities compounded by issues of poverty, racism, and access. This is true regarding food insecurity and access to healthy food.
Amongst its many strengths, the community has a history of building strong partnerships and utilizing an asset-based approach to identify and leverage existing community resources to address community health concerns. These elements are evident in the innovative strategies Spectrum Health employs to address the pressing health needs in their community.
Organization of community benefit and community health activities
Spectrum Health has a system-level steering committee that oversees community health needs assessments (CHNAs) and guides the development of community benefit implementation strategies. This committee largely consists of staff members with roles and responsibilities within the corporate system that supports Spectrum’s health plan, medical group and 12 acute care hospitals, including the vice president of Spectrum’s Healthier Communities program, staff from human resources, corporate finance and others. At the system level, this committee determined all Spectrum hospitals would address “access to care” and one or two other priority health issues based on the needs of their respective community.
Each facility has a working committee that is coordinated by the hospital group president. This committee is responsible for defining what “access to care” means in their specific community and works together to select additional priority health needs and intervention strategies.

Community health needs assessment: Priorities and process
- Food and diet-related disease priorities:
- 2014 CHNA - Obesity, poor nutrition
- Participation from food-based organizations in CHNA process
- Feeding America of West Michigan, Eastern Avenue Food Bank, Food Security Advocate, Our Kitchen Table, Kent County farmers markets, Access of West Michigan, and area restaurants
- How/why did food issues emerge as a priority?
- Multiple evaluations from credible sources, including the Kent County CHNA and national INVEST HEALTH initiative, reported high obesity and poor nutrition, especially in youth populations, as key areas for improvement
- Key community indicators
- Obesity rates in Kent County have been climbing steadily, up 11% since 1993
- 28.8% of middle school to high school-aged youth are considered overweight, and 21.1% are considered obese
- Less than one-third of middle school to high school-aged youth report eating the recommended daily servings of fruits and vegetables
Full assessment: Kent County Community Health Needs Assessment
Assessing health needs—and how to meet them
Community health needs assessment process
For over 20 years, government, hospitals, and a wide array of community organizations in Kent County have come together under the banner “Healthy Kent.” In 2013, Healthy Kent took on the role of convener for the second countywide community health needs assessment (CHNA), with the Kent County Health Department (KCHD) at the helm. The department convened over 128 organizations with expertise ranging from food security to housing and seven health care facilities, including Spectrum Health, to participate in a collaborative CHNA process.
Health department staff members began the 2014 Healthy Kent CHNA process by reaching out to a list of key community partners, particularly nontraditional partners, and community sectors that were missing from the previous countywide CHNA process to establish a more inclusive process.
Food-related organizations including Feeding America of West Michigan, Eastern Avenue Food Bank, Food Security Advocate, Our Kitchen Table, Kent County Farmers Markets, and area restaurants engaged in data collection, review and needs prioritization activities by participating in or supporting community health forums, community health surveys, and Healthy Kent Summit activities. This engagement led to a more comprehensive view of needs as a result of more expansive data collection with contributions from thousands of residents and multiple sectors of the community.
An extensive data collection and analysis process was managed by an epidemiologist from KCHD with support from community organizations. A community health survey included questions about access, availability, and affordability of healthy food; nutrition and healthy skills education; diet-related diseases; and food insecurity.
Community food system partner organizations played an instrumental role in survey success by conducting targeted outreach to their service recipients and collecting survey responses. Organizations working on food access and food insecurity participated in numerous community health forums to identify strengths, weaknesses and health concerns, thus ensuring that food-related elements were represented in the assessment of community health assets and concerns.
Obesity and poor nutrition were among four priority health needs selected by the community and adopted across the board at each health institution participating in the collaborative CHNA.
Each institution determined which needs they wanted to address in their community benefit activities and how to do so. For Spectrum Health Grand Rapids hospitals, a focus on food was obvious. Obesity rates had been steadily increasing for over a decade and fruit and vegetable consumption among middle and high-schoolers was remarkably low. Furthermore, extensive past experience with food and diet-related programming made these strategic intervention points.
— Ken Fawcett, Spectrum Health vice president of healthier communities
Investing in solutions
Implementation strategy
In response to the region-wide CHNA findings, Spectrum Health has made significant investments of staff time, in-kind resources, and grant funding to programs working to address food insecurity and diet-related disease in Grand Rapids, Kent County and beyond. Spectrum has partnered with Access of West Michigan to run a food pantry-based Nutritional Options for Wellness (NOW) program since 2004 and provides financial and in-kind support to the Community Food Club of Grand Rapids – a community partner piloting an innovative membership-based community grocery store model.
Nutritional Options for Wellness
A food-pantry-based lifestyle medicine program with the aim of promoting self-management of chronic disease and supporting increased wellness through education, healthy food, social connectivity, coaching, and goal-setting support.
- Program type: Produce and healthy living prescription program
- Program administrator: Access of West Michigan
- Program founded: July 2004
- Hospital role: Provide grant support, conduct nutrition education, provide staff support for developing nutritionally appropriate food options.
- Community partners: Spectrum Health, seven community centers, food pantries, local small farms, more than 40 local primary care physician offices, healthy living class educators
- Population served: Low-income adults with chronic disease
- Program goals: Improved chronic disease self-management; increased healthy eating, shopping and cooking skills; increased healthy lifestyle behaviors; and decreased social isolation
- Health needs addressed: Obesity and poor nutrition
- Key outcomes:
- 97% of program participants reported that their overall health improved
- 70% reported fewer visits to the Emergency Department
- 90% reported that they are cooking healthier for their families and friends
- 2,777 healthy food and coaching services provided
- Over $16,000 invested in fresh produce from local farms for distribution to NOW participants through local food pantries
Project description
The Nutritional Options for Wellness (NOW) program provides healthy foods, healthy living classes, and connections to other community food resources to low-income adults with a chronic health condition upon referral by their primary care physician. Distinct among healthy food prescription programs NOW provides medically appropriate food tailored to an individual’s chronic health needs. The goal is to nurture healthy habits through nutrition, cooking, and exercise classes for individuals and their families. The program provides participants with the resources they need to successfully manage their disease and reduce disease risk factors.
The Nutritional Options for Wellness program was created by Spectrum Health in 2004. Since 2013 the program has been administered by Access of West Michigan, a community-based organization in Grand Rapids. Access performs fiduciary, administrative, fund development, and reporting functions for NOW and provides support, training, and program monitoring to seven community centers/food pantry partners that operate the program in diverse neighborhoods throughout Kent County.
Primary Care Physicians from over 40 local medical offices affiliated with various health systems refer eligible patients to the NOW program. The team at NOW assigns each patient to one of seven community partner sites based on their location for a one-year term in the program. Patients visit the site weekly to receive three to four days worth of highly nutritive, plant-based food that fits their specific chronic disease dietary needs.
Participants are required to attend healthy lifestyle classes throughout the year, which are focused on four education modules: nutrition and affordable food sourcing, cooking and gardening, disease education, and healthy movement and stress management. Each site hosts classes and has a coordinator who works with participants to set goals related to each education module, checks in on progress and challenges, and offers coaching and support. At the end of the year, patients are connected with a volunteer peer mentor or coach to provide support for maintaining healthy behaviors without the supplemental food or structure provided by the program.
The program also helps individuals and the NOW sites to make mindful decisions about food sourcing. Access works with the NOW sites (and other community partners) to set nutrition standards, implement product placement and promotion strategies to encourage healthy choices, and helps the sites provide local, organic produce to clients through connections to local farms and financial support for farm fresh produce. Program participants can also fulfill one of the NOW curriculum module requirements by taking gardening classes, providing them with the tools to grow their own healthy foods.
Program participation
Low-income adult patients (age 18+) diagnosed with type 2 diabetes, cardiovascular disease or renal disease are eligible for the NOW program. Participants learn about the program through participating primary care physicians (PCP), affiliated community-based organizations, word of mouth, or local and social media. The actual referral must come from a PCP.
To participate in the program individuals must commit to:
- Complete 16 hours of healthy living education (four hours per quarter within the four topic modules)
- Connect weekly with NOW Coordinator to update goals and receive healthy food supply
- Complete program participant survey five times (baseline, and every three months through completion of program)
- Submit initial lab data and return to primary care office at end of program for follow-up lab data
- Participate in coaching/mentor element after one year program period
The NOW program is not the right fit for all patients meeting eligibility criteria. Successful participants have reliable transportation and are interested in – and willing to commit to – making a long-term lifestyle change. Access conducts education with PCP offices each year to help them identify and refer appropriate candidates.
Through the NOW program, Access currently provides more than 200 low-income community members with healthy food and health education on a weekly basis. Participants reported improvements in overall health and healthy behaviors, including significant physical and lifestyle changes. Participants go through the program as part of a cohort and express the value of connection and support – reporting benefits such as decreased social isolation, improved emotional health, overall wellness, and vibrancy.
Partnerships and hospital role
Spectrum Healthier Communities staff ran the program and partnered with Access to help connect patients with local food pantries. In 2013 program administration transferred to Access of West Michigan because in the words of Dr. Ken Fawcett, vice president of Spectrum Health Healthier Communities, “they could run a pantry system better than we can.”
Access of West Michigan employs a part-time program manager and project coordinator to manage the program and hosts dietetic, public health, social work, biomedical science, and nursing interns from Grand Valley State University, Davenport University, and Calvin College to help manage program referrals and connect with PCPs.
Seven local community centers/food pantries serve as NOW sites. Each site provides a staff member that commits at least 10 hours per week to the NOW program to manage food procurement and distribution, coordinate classes, provide coaching and support to participants for goal setting and resource referral.
Access works with community partners including Spectrum dieticians, Michigan State University Extension educators, the local YMCA (which offers Cooking Matters curriculum), and other community agencies that have funding to do SNAP-Ed (Supplemental Nutrition Assistance Program-Education) to provide healthy living classes at NOW sites.
Spectrum provides funding and in-kind personnel support for the NOW program, including:
- Spectrum Health primary care offices and physicians participate in recruitment by making patient referrals.
- Spectrum dietitians and community educators helped shape the overall process, deliver healthy living classes, and help develop nutritionally appropriate menus.
- The data and analytics team within Spectrum’s Healthier Communities program provides guidance and advice as needed regarding program evaluation and data analysis.
“Overall Spectrum’s partnership is incredible. They are deeply involved in the community and are passionate about addressing health inequity. We’ve valued their ability to not only provide financial support for the program, but also practical on-the-ground support to make it successful.”
— Emma Garcia, Access of West Michigan co-executive director
Access also partners with six to seven small local farms to connect NOW food pantries with fresh, local produce. Access purchases community-supported agriculture (CSA) shares for each of the NOW sites. According to Emma Garcia, Access of West Michigan co-executive Director, “That’s a weekly supply of farm fresh food, mostly organic, and those healthy vegetables go directly to the participants while payment to our farm partners invests in creating a more resilient and robust local food economy, creating jobs and thereby preventing poverty.”
Financing
Access receives funding from Spectrum Health through an annual grant process. Spectrum funding supports program administration staff at Access, some indirect costs that Access and host organizations incur, part of the staff time contributed by each host site, and all food costs.
The yearly grant from Spectrum does not cover total program cost. Some of the host organizations obtain additional, smaller grants to support the program at their location and each contributes a significant amount of in-kind resources including staff time, volunteer hours, and materials such as cooking supplies. The education classes and peer mentorship/coaching that occurs also rely on in-kind staff time. Access is working with NOW sites to begin tracking and collecting this information so they can more accurately capture and communicate the true cost of the program.
Program evaluation and impacts
Spectrum’s Healthier Communities department includes a four-person data and analytics team that helps Access define metrics, develop evaluation plans and data collection tools, and inform data analysis. Access is also working with this team to explore developing a system to support a shared data collection, outcomes, and metrics dashboard with other community programs.
Access of West Michigan manages data collection, analysis and reporting for the NOW program. They track impacts on individual health outcomes through health data provided by PCPs and participant surveys. Access receives a lipid panel with lab values for each participant upon referral from their PCP, and follows up with panels one year later at program completion, and again when the patient has been out of the program for a year. Comparison of weight, body mass index, blood pressure, cholesterol, A1C values, and other indicators from beginning to end of the program and one year later are used to help identify health impacts and determine if changes are sustained.
Pre- and post-program participant surveys are administered to gather data on: improved disease self-management; increased healthy eating, food preparation skills, and healthy lifestyle behaviors; decreased social isolation; and reduced recourse to emergency care and hospitalizations due to chronic disease.
Evaluation has informed a number of program changes over the years. Most recently, Access refined and standardized education modules, and reduced the program length from two years to one year based on program retention trends and behavior change research literature. Additionally, Access has moved to a whole foods framework grounded in evidence-based research demonstrating the impact of a plant-based diet to reduce and even reverse disease symptoms.
The NOW program has been remarkably successful by all available metrics. In 2016, there were 231 participants. Of participants surveyed:
- 97 percent reported that their overall health improved
- 95 percent felt better about self-managing their disease
- 70 percent reported fewer visits to the emergency department
- 90 percent reported that they are cooking healthier for their families and friends.
Additionally, the NOW program invested over $16,000 in fresh produce from local farms for distribution to NOW participants, provided 2,777 healthy food and coaching services, and provided 603 hours of education through Healthy Living Classes.
Cooking up lifelong change
Clients experience benefits on a number of levels. Connie, a NOW client with type 2 diabetes was facing the likelihood of blindness and loss of a limb without a lifestyle change. After a few months of weekly groceries and participation in NOW Healthy Living classes, management of her condition improved significantly as did her quality of life and mental health.
“I’ve lost 28 lbs. and my A1C is down to 6.9. It has been at 8.1 for years,” she told her local food pantry. “I have more energy and less depression. The NOW program is the best thing I’ve done… my best friend is now enrolled too.”
In addition to improved health outcomes and health behaviors, Spectrum has seen significant improvement in the way their patients are using the health care system.
“These underserved patients often use the emergency room to treat their chronic diseases, however, since the NOW program began in July 2004, among patients who participate in the NOW program there are 25 percent fewer emergency room visits and a 44 percent decrease in the number of hospitalizations.”
— Mary Kay Kempker-VanDriel, former Spectrum Health healthier communities director (currently president of Big Rapids and Reed City hospitals)
Currently, Access is working to demonstrate the impacts of a reduction in ER visits and hospitalizations to build a case for health care savings as a direct outcome from the NOW program. Access is seeking to connect with insurance partners and is learning from healthy lifestyle intervention programs across the country to inform a platform for evidencing cost savings and a case for insurance rebates and reimbursement.
Lessons learned
Emma Garcia, Access co-executive director’s advice is to “listen to the community. Take the time to both know the end users and also the entities that are helping shape or carry out the programming.” She underscores the importance of strong, trust-based partnerships with the community and genuine collaboration. “Often programs will set themselves up without any feedback from the community and without evaluating health inequities from the community’s perspective,” Garcia said. “They’ll just strike out and say ‘we think this is a need, let’s start this up!’ I caution against that.”
Access took a different approach, they went directly to the NOW pantries and asked what they were seeing and hearing, and how they thought the program could be changed and improved.
Building strong relationships with community partners from the outset by taking time to ask questions, listen, recognize, and value their expertise by engaging them as partners in shaping the program is essential for long-term success.
Garcia explains that they’ve “had to have a lot of hard conversations over the four years with our partners.” Trusting relationships gave them the ability to confront issues, navigate conflicts, and successfully execute collaborative programs.
At the same time, Garcia admits that Access’s expertise lay in organizing, convening, and connecting; the medical side was foreign to them. Recognizing this, being willing to do the research and make changes was key. Garcia explains, “We’ve had to make very drastic changes based on evidence-based research and expertise from the medical field.” Each partner brings unique value and expertise to the table. Recognizing and honoring this, being open to learning and changing the way one typically operates on all sides is what makes for strong, successful programs and partnerships.
The Community Food Club
Provides a systematic response to hunger for low-income families by promoting food security, consumer choice, and dignity in a grocery store environment.
- Program type: Community food retail warehouse provides healthy food resources to low-income club members.
- Program administrator: Seven community organizations collaborated and established Community Food Club (CFC) as a limited liability company. The company functioned as a separate entity with Home Repair Services (HRS) as the fiduciary and employer of record. The Food Club is operated by its own staff and governed by a board of directors.
- Program founded: 2014
- Hospital role: Provide grant support
- Community partners: Home Repair Services, Feeding America, Access of West Michigan, Habitat for Humanity, Salvation Army, Westminster Presbyterian, Southeast Community Outreach Ministries
- Population served: Families with incomes below 200 percent of the federal poverty level who receive services from one of the seven parent organizations.
- Program goals: To provide food access in a dignified shopping environment for low-income families and incentivize healthy consumer behavior.
- Health needs addressed: Obesity and poor nutrition
- Key outcomes:
- More than 1,700 households received access to nutrient-rich food options.
- Customers are highly satisfied with the novel shopping environment: 25 percent never return to a food pantry.
- Fresh produce represents 35 percent of sales, about twice as much as in a traditional grocery store.

Program description
The Community Food Club of Greater Grand Rapids is a food retail warehouse combined with a consumer membership model designed to increase food security, consumer choice, and dignity for low-income households.
In 2012, seven community agencies serving the Greater Grand Rapids community came together to discuss a growing crisis: many local families regularly struggled to put food on the table. Food pantries did great work but were overburdened and food insecurity rates continued to rise. Kent County had more than enough food to help prevent the monthly crisis experienced by many food-insecure residents. This group of community partners believed there could be a different model, one that took a more proactive approach.
Determined to create new opportunities for residents who sought greater food security, these partner agencies committed to bringing new choices and dignity to the experience and embarked on a collaborative planning process.
The doors to the Community Food Club opened in the winter of 2015. Partners repurposed existing warehouse space located along a major bus route in an area that lacked healthy food options and created a vibrant, innovative, affordable food outlet designed to increase food security and reduce reliance on emergency food resources.
The club offers an opportunity and a place for households to increase their food security and improve their healthy eating by accessing nutritious food on a consistent basis. The consumer is at the center of the entire operation. This collaborative, systemic response to hunger attempts to provide an experience that may be transformational for the consumers.
Low-income residents pay a small monthly membership fee to participate in the club. For $10 a month, members receive points based on their household size to shop in a welcoming grocery store style environment where consumer choice and experience is a priority. The club is open six days a week, with convenient daytime and evening hours, and offers a wide selection of high-quality food items, including fresh and nutritious products. Members can shop as often as they want each month to spend their allotted points and are guaranteed to find certain products in stock every day such as fresh produce, milk, cheese, eggs, and meat.
The club encourages healthy choices by employing pricing, promotion, and environmental strategies. They turn the tables on pricing by making healthy foods the least expensive — produce costs one point, while processed food items high in sugar and fat costs four points.
The club also provides opportunities for members to learn together by hosting facilitated discussions on topics such as meal planning and healthy eating on a budget and by offering a series of classes on basic nutrition and healthy cooking in their on-site teaching kitchen.
Program participation
Community members are eligible to participate in the Community Food Club if they earn less than 200 percent of the federal poverty level. The club seeks to assist households whose:
- Needs are not adequately met via emergency food pantries
- Earn below 200 percent of the federal poverty level and are not eligible for most government assistance;
- May receive public benefits, but additional supplementation is needed to ensure there is enough food for an active, healthy lifestyle.
Most members are referred to the program through a partner agency, or learn about the program by word of mouth through social networks and verify they meet eligibility requirements during screening.
Partnerships and hospital role
The Community Food Club is intentionally collaborative in nature and design. Seven local organizations came together and established the club to test a collaborative, systemic approach to addressing hunger and improving food security.
Founding partner agencies included: Westminster Presbyterian Church (Downtown food pantry); United Church Outreach Ministry (UCOM); the Salvation Army Social Services; Feeding America - West Michigan Food Bank; Habitat for Humanity Kent County; Home Repair Services of Kent County; Access of West Michigan.
Administrative staff was hired to run the Community Food Club. Three full-time staff members – an executive director, grocery manager, and assistant program manager – coordinate and manage the program. Two part-time employees help run the floor and assist clients with the support of volunteers from local churches, colleges, and community organizations.
During the first three years, the collaborative operated as a Limited Liability Company. Now at the end of the three-year pilot phase, the Community Food Club decided to continue operating and is working to establish itself as an independent nonprofit organization.
The Food Club was built on the strengths of partner agencies — each offered unique resources and expertise and was instrumental in establishing the program. Home Repair Services shares a building with the Food Club and served as fiduciary for the pilot. Westminster Presbyterian provides volunteers and manages the website. The club purchases 50 percent of its food through Feeding America. Salvation Army provides the majority of program referrals and handles intake - processing referrals, verifying household income, and putting new members into the computer system. This support creates an efficient process, is essential to maintain a manageable workload for Food Club staff, and intentionally removes any sense of receiving benefits or social service support from the Food Club. When new members arrive at the club they simply pay the $10 fee and start shopping.
Spectrum Health is the largest funding source. They provide program referrals and play an important part in raising awareness about the program. Spectrum also provides staff support regarding evaluation and metrics and through their work to explore a shared dashboard for measuring community impact.
“When people hear Spectrum Health is our partner it gives us credibility. Particularly when it comes to health — Spectrum staff helps the Food Club team understand health impacts and benefits, and provides guidance to help shape the program.”
— AJ Fossel, Community Food Club executive director.
Financing
In 2016 the Food Club budget totaled $441,652. Funds come from three major income streams. The Food Club uses a membership model which both provides revenue to support operations and provides consumers with dignity in their shopping experience. Membership fees account for approximately one-quarter of program revenue ($92,000 in 2016).
Foundations and community organizations provide the majority of funding; numerous individuals and corporations also make contributions. In 2016 the Food Club had 76 financial supporters, raising a total of $349,012. Spectrum Health provides general operating funding that covers the majority of food costs (around 75 percent) and supports staffing and evaluation. The club also receives significant funding through an ongoing partnership with United Way and from the Kent County Senior Millage, which provides funds to cover program costs for participants 60 years of age and some operational expenses.
Program evaluation and impacts
The Community Food Club was designed as a three-year pilot project to test effectiveness and efficiency of this model and its overall impact. The Food Club worked with the Johnson Center Community Research Institute of Grand Valley State University for program evaluation, which included identifying goals and outcomes, as well as designing and implementing a formal evaluation plan.
Program goals included:
- Increase food security for low-income households who join the Food Club
- Increase member households’ empowerment, dignity, and self-reliance through the Food Club
- Improve healthy living by accessing nutritious food choices on a consistent basis
Data is collected through member surveys completed at the point of registration and every six months. Surveys gather information about participant experience, satisfaction and behaviors such as eating habits and use of emergency food resources. Periodic member focus groups are held to gather feedback used to shape and improve the program.
Additional data is collected by monitoring indicators such as clients served, number of checkouts by members (to identify shopping trends), pounds of food distributed, items sold by category (produce vs. processed), total food purchased by the club each month and cost per point of food. The computer program developed to manage Food Club membership and operations is linked to the checkout payment system and helps manage analytics for this data.
In 2016, during its second year of operation, the Community Food Club:
- Welcomed 2,086 member households, for a total of 2,505 since opening in 2015
- Engaged 130 community volunteers, who provided 2,765 hours of service
- Distributed an estimated $801,000 worth of food
- Grew to become the single highest food distribution outlet within Feeding America West Michigan’s 40 county territory
- Sold almost twice as much produce as a traditional grocery store, fruit and vegetables represented 35 percent of grocery items selected by member households
Participant survey results indicate many positive impacts. After 12 months of membership in the Food Club:
- 79 percent of respondents stated: "My family and I eat more fruits and vegetables now than we did before we joined the Food Club"
- 24 percent of respondents did not return to a pantry, mobile pantry or free community kitchen in the last six months
- 31 percent of respondents reported an improvement in their ability to meet their basic needs
- 26 percent of respondents reported an improvement in the health of their diet
“I realized some benefits right away but as I made future trips I started to feel a real impact on my life and budget - I was able to allocate my funds better as a result of this program. There were many times I wasn’t sure how I was going to make it. I go to the Food Club before any other store so that I can get the healthiest food for my family… The Food Club has helped ease my burdens so many times. I always feel so welcomed and never feel embarrassed to come in or as I leave. Although I’m in a time of need I always leave with my pride and dignity intact and feel uplifted after I’m there. I don’t know what I would do without [this program]!”
— Amber, Community Food Club member
Members share that the Food Club eases financial stress because they are able to redirect limited resources to pay off other bills and meet other basic needs. Many participants also note a meaningful effect on self-esteem and express gratitude for the fact that that this model provides the opportunity for them to make healthy choices without compromise — the Food Club allows and empowers them to become actively engaged in determining their health.
"I can come to the Food Club monthly, as I do, feeling good that my family is being taken care of. It meets our household’s desire to lead a more healthy lifestyle with more fresh vegetables and healthy foods — a goal of ours and the point system allows us to achieve this goal at an even greater level. Buying fresh can be very expensive — especially when one is low-income."
— Tom, Community Food Club member
In the future, they would like to connect program evaluation with patient medical record data. Dr. Ken Fawcett, Spectrum Health Healthier Communities vice president explained, “I have stories, anecdotally, where people have been able to come off a hypertensive medication, diabetic medication, because they are eating a more healthful diet. At this point, we have not incorporated those as outcome measurements but we hope to be able to do so.”
Evaluation has informed a number of small program implementation changes with big impacts, such as adjusting the point structure and allocation formula because the survey data indicated larger households were not receiving enough food. Monitoring sales by food group provides real-time data about what members want to see on the shelves and staff can adjust purchasing accordingly — producing happier customers, less waste, and a more efficient system.

Lessons learned
Having members pay some amount is crucial. This personal contribution creates buy-in, which is a fundamental ingredient for success in this model and key for fostering a sense of community.
Member participation in shaping this community program has always been a priority. This is significant because successfully operating a grocery store requires knowing what people want, what they are willing to pay for different items, and responding to member needs and desires. Staff experimented with point allocation and pricing structure in order to find a system that worked. In addition to lending their voices through regular surveys, Food Club members participate in focus groups and serve on the board of directors. Food Club staff also closely monitor sales data to identify what products are most popular and can adjust purchasing, pricing or promotion accordingly. This consumer-centered approach with multiple feedback mechanisms is key for success.
Fossel underscores that “you can never have enough quality data.” From day one the team worked with the community research institute at Grand Valley, to clearly define goals and develop good evaluative tools to produce strong data. The data and member’s stories clearly illustrate the impact of the program — particularly for funders — and also guide general program growth and development. Fossel encourages others to work with data management experts and to start planning for evaluation early in order to establish effective, efficient systems and processes.









