Program: School lunch and breakfast
Takeaways
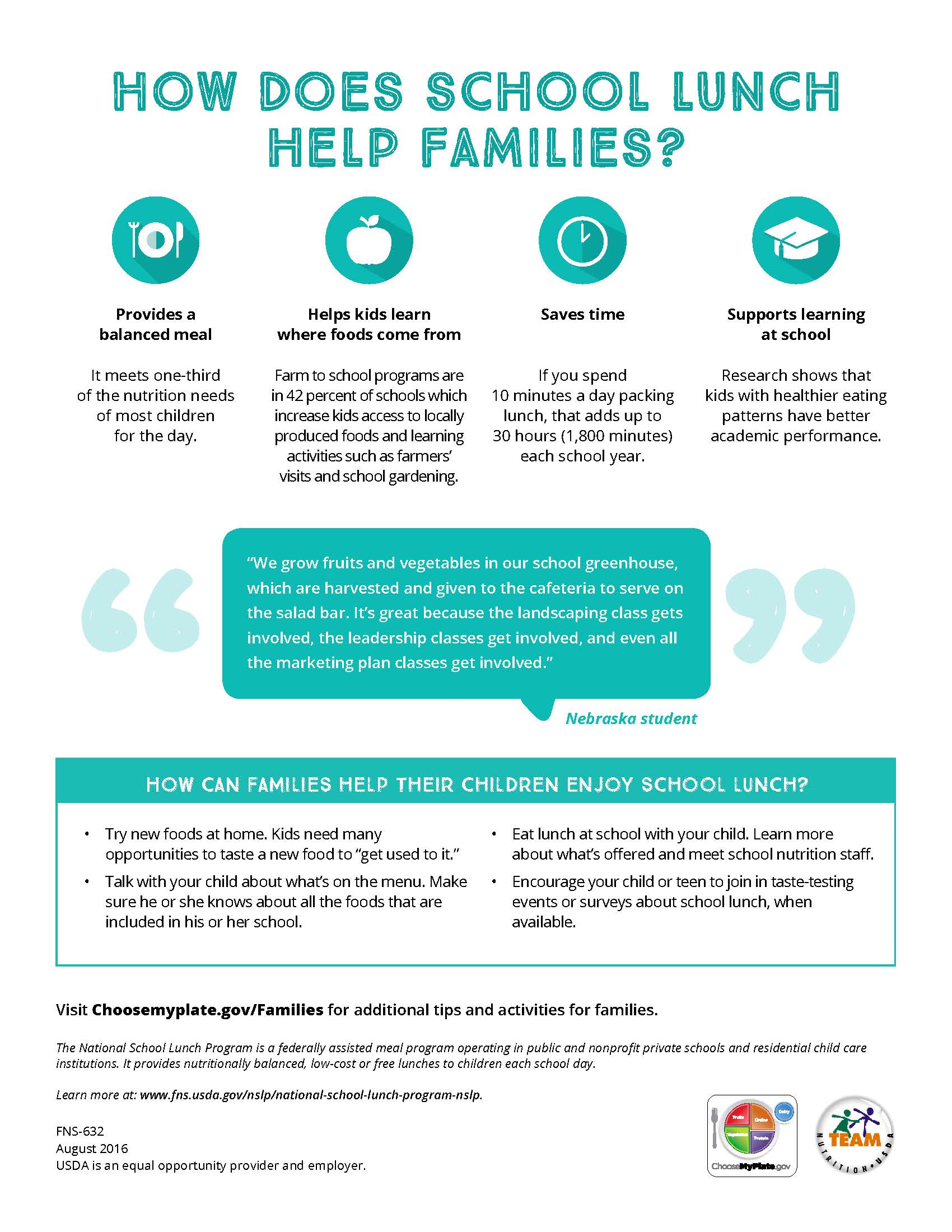
- This brief describes federally subsidized school meal programs, which are an integral source of food and nutrition for millions of students across the country, particularly children from low-income households.
- School meal programs offer meals meeting dietary guidelines, create an opportunity to educate students on food, nutrition, and health topics, and are vital in addressing food insecurity and promoting healthy eating behaviors for school-age children.
- The brief offers recommendations and examples for how hospitals can provide community benefit support to enhance the reach and impact of school meal programs.
- Schools face significant time and financial constraints in implementing school food environment changes, and hospitals can be valuable partners in establishing policies to guide changes, facilitating staff training and infrastructure updates to make changes, and enhancing food and nutrition education efforts.
- Schools face significant time and financial constraints in implementing school food environment changes, and hospitals can be valuable partners in establishing policies to guide changes, facilitating staff training and infrastructure updates to make changes, and enhancing food and nutrition education efforts.
Each day tens of millions of children and youth rely on federally subsidized school meals. These programs, administered by the United States Department of Agriculture’s Food and Nutrition Service (USDA-FNS), operate in every community in the country. While school meals are an important safety net for children from low-income households, all students benefit from efforts to promote healthy food choices and increase access to nutritious food. Rooted in the Dietary Guidelines for Americans, these programs promote students’ health and development by improving food access and encouraging healthy behaviors. Program objectives align closely with those pursued by hospitals and the strategies recommended by the Centers for Disease Control and Prevention (CDC) to treat and prevent obesity and diet-related disease and to promote community-wide food access.
Value of school meals
The USDA’s National School Lunch Program and School Breakfast Program are designed to ensure children have access to nutritious, school-based meals. The school lunch program operates in more than 100,000 schools nationwide and serves more than 30 million students daily. The breakfast program runs in more than 87,000 schools and serves approximately 14.6 million students daily. Children from low-income and food-insecure households, in particular, depend on these meals for a large portion of their food needs. More than half of public school students in United States schools are from low-income households, and 13 million children live in food-insecure households. Free and reduced price meals made up approximately 75 percent of the 5 billion lunches served under the program in 2016, an indication of the importance of this program to families.
Students are a captive audience, making schools a good environment for influencing eating behaviors and encouraging positive changes that have long-term health impacts. Research findings demonstrate the value of school meal programs in supporting children’s health:
-
Research indicates participation in or availability of school meals contributes to lower rates of household food insecurity for children.
-
Students who participate in school meal programs eat more fruits and vegetables and have a higher intake of calcium and fiber than peers who do not eat school meals.
-
Students who participate in farm-to-school activities, which enhance school meal programs, demonstrate increased food and nutrition knowledge, a willingness to try nutritious foods, and improvements in fruit and vegetable consumption.
Healthy eating behaviors and access to nutritious food also support academic achievement. Research indicates there is a connection between the presence of a school breakfast program and higher academic achievement and improved behavior. While changes to nutrition standards have aimed to improve the quality of school meals to support improved health outcomes, a 2017 California-based study concluded that improving meal quality could also be a cost-effective way to boost students’ academic achievement.
USDA school breakfast and lunch programs
School breakfast and lunch programs are part of the USDA’s larger child nutrition programs portfolio and involve coordinated efforts on the federal, state, and local level. State agencies partner with USDA Food and Nutrition Service, with specific support from USDA regional offices, to administer the programs. Local school authorities carry out the program in accordance with state and federal guidelines. Public and private nonprofit schools for grades 12 and under can participate in these programs. Participating schools receive reimbursement for each meal served and can access commodity foods, including meat, poultry, eggs, cheese, fruits, and vegetables, to offset cost.
The federal government (via state agencies) reimburses participating schools for lunch and breakfast meals served, based on the types of meals sold (free, reduced, full-pay), with the reimbursement amount decreasing as ability to pay increases. In the 2017-18 school year, federal reimbursement ranged from $3.23 for free lunch to 31 cents for fully paid lunches, with an additional reimbursement available for commodity foods and in accordance with particular school circumstances (e.g. high percentage of meals are free or reduced price). State and local authorities may contribute additional funds to fill budget gaps, but deficits often persist. Federal, state and local funding goes toward food, overhead, and administration. In the end, after other expenses, the funds available for food can be as limited as $1 per meal.
School breakfast participation rates lag lunch participation rates significantly, with only half the number of eligible students taking part. The “breakfast after the bell” approach aims to increase program participation by moving breakfast service from the cafeteria (before the school day starts) to the classroom (as part of the school day). Various models of breakfast after the bell exist, including grab-and-go, breakfast in the classroom, and second chance, and all share the common objective of making breakfast more convenient and accessible for all students. Hospitals can support these efforts by helping schools secure funding to implement these models or by giving financial support to fund program and equipment changes, such as the acquisition of carts and coolers to make it easier to offer breakfast outside of the cafeteria.
The Community Eligibility Provision offers a new reimbursement model for schools. Under this provision, schools and/or districts in low-income communities can offer universal free meals when more than 40 percent of their students are enrolled in Supplemental Nutrition Assistance Program and other benefit programs. Across the participating schools, the community eligibility program gives more than 9 million students free access to breakfast and lunch and increases breakfast and lunch participation. Yet only half of the eligible schools take part. Hospitals can find out if local schools are eligible for and enrolled in the community eligibility program through the USDA website. For eligible schools that are not enrolled, hospitals can make sure schools are aware of the opportunity, advocate for participation, and work with schools to facilitate the application process.
Healthy, hunger-free kids
The Healthy Hunger Free Kids Act of 2010, a reauthorization of the Child Nutrition Act, instituted new nutrition standards for USDA-reimbursed meals and new policies and procedures to improve the overall quality of food service in an effort to more aggressively address the country’s obesity epidemic. With nearly 20 percent of school-age children in the United States classified as obese and Americans of all ages under-consuming fruits, vegetables, and whole grains (while over-consuming fats, sodium, and sugar-sweetened drinks), Healthy Hunger Free Kids established a multi-pronged approach to address eating behaviors, nutrition knowledge, and school food environments. This legislation called for increased technical assistance and training for food service staff to make it easier to create healthier menus and established the use of evidence-based standards for snack offerings, a la carte items, and vending machines. Nutrition standard changes specifically sought to decrease over-consumption of low-nutrient-density foods, such as potato chips, sugar-sweetened drinks, and baked goods. Research indicates changes have positively influenced students’ nutrient intake and improved the quality of school meals.
Nutrition and health education are key components of USDA-FNS programs. The USDA’s Team Nutrition specifically focuses on child nutrition and uses a communications and education strategy in both cafeterias, classrooms, and the community. For instance, Team Nutrition produces a variety of kid-friendly materials to make healthy food appealing and to encourage healthy eating behaviors. Messaging for students and caregivers relays information on healthy eating and on how to create healthy meals. Technical assistance and training activities support food service professionals in creating healthier meals.

New York hospital builds strong foundation for healthy eating in schools
Glens Falls Hospital works with five school districts in a rural area of upstate New York. With funding support from the New York State Department of Health Creating Healthy Schools and Communities Initiatives, the hospital coordinates comprehensive programming to support school-based health. The hospital’s efforts to promote quality nutrition in schools focus on offering technical assistance, professional development, continuing education, and learning resources to ensure school district staff have the knowledge and skills to create healthier food environments. Collateral support provides salad bars, food carts, and other kitchen equipment to make it easier to serve fresh, nutritious options. The hospital also supports school wellness committees and the development of district wellness policies that improve the school food environment, such as healthy vending and healthy fundraising opportunities (e.g. fruit and veggie box sales rather than candy bars).

Orange Center Elementary School’s Healthy Living Garden creates an interactive venue for teaching students about good food choices and for promoting overall health and wellness (Orlando Health).
Recommendations for hospital community benefit engagement
School meal programs present an opportunity for hospitals to support well-established efforts that have been proven effective in promoting children’s health and in alleviating food insecurity. There are many opportunities for hospital engagement and support.
- Hospital staff can contribute nutrition and policy expertise to help school districts develop wellness strategies that support healthy eating behaviors, such as healthy vending and eliminating sugar-sweetened beverages.
- Hospital staff can also help create curricula and learning opportunities related to nutrition, health, and food to complement USDA efforts. Curriculum can integrate food and nutrition into core subjects (e.g. math, science), creating new and engaging learning opportunities.
- Through financial support, hospitals can increase the capacity of school programs to serve healthy, fresh food and to make program changes designed to increase student participation. Many schools lack sufficient funds to purchase healthier foods and also the infrastructure and skilled labor to handle fresh foods. For instance, offering salad bars is an effective way to increase fruit and vegetable intake, but many schools cannot afford the implementation investment. Specific examples of hospital engagement to support school-based meal programs are outlined below.
Examples of hospital roles and participation
Cheshire Medical Center Dartmouth-Hitchcock, N.H. (Coordinate community coalition to enhance capacity of schools)
Coordinate community coalition to enhance capacity of schools to serve high quality of meals
![]() Cheshire Medical Center Dartmouth-Hitchcock
Cheshire Medical Center Dartmouth-Hitchcock
Keene, N.H.
Healthy Monadnock
Healthy Monadnock, a coalition coordinated by the hospital, has engaged 25 school champions and supports their efforts with funding, resources, and direct staff support.
Through its mini-grant program, Healthy Monadnock supported nutrition education and physical activity for eight school and afterschool programs, reaching 1,029 students.
Orlando Health, Fla. (Conduct nutrition/food/cooking education)
Conduct nutrition/food/cooking education
Orlando Health
Orlando, Fla.
Orange Center Elementary
Staff conduct nutrition and food education classes at elementary school and engage students in Healthy Living Garden.
Entire student body (345 students) participate in planting and harvest events and monthly nutrition education sessions, based on grade-appropriate curriculum.
Northwestern Medical Center, Vt. (Conduct nutrition/food/cooking education)
Conduct nutrition/food/cooking education
![]() Northwestern Medical Center
Northwestern Medical Center
St. Albans, Vt.
select Franklin and Grand Isle County schools
Northwestern Medical Center’s RiseVT initiative provides grade-specific nutrition and health education to participating schools.
RiseVT works with a total of 18 area schools and offers classroom resources addressing healthy eating and active living for grades K-8.
University of Vermont Medical Center (Provide financial/grant support)
Provide financial/grant support
![]()
![]() University of Vermont Medical Center
University of Vermont Medical Center
Burlington, Vt.
Hunger Free Vermont
Through its Community Health Investment Fund, University of Vermont Medical Center supports Hunger Free Vermont’s efforts to expand breakfast in schools across the state.
Hunger Free Vermont’s Breakfast after the Bell Challenge engages schools to increase breakfast participation by 20 percent. Thirteen schools succeeded in doing so in 2016. The challenge winner had a 642 percent increase in participation.
Glens Falls Hospital, N.Y. (Provide financial/grant support)
Provide financial/grant support
Glens Falls Hospital
Glens Falls, N.Y.
five school districts
Glens Falls Hospital works with five school districts in rural upstate New York, providing technical assistance to help improve the school food environment. The hospital also provides equipment, such as salad bars and gardening equipment.
Glens Falls has donated equipment for salad bars to five schools, giving students increased access to a variety of fresh fruits and vegetables at lunch.
Valley View Hospital, Colo. (Contribute materials/equipment)
Contribute materials/equipment
Valley View Hospital
Glenwood Springs, Colo.
Two Rivers Community School
Donated kitchen equipment (valued at $100,000) to Two Rivers Community School, which previously had no cafeteria.
228 students in K-12 charter school now have access to the USDA school meal program.
Learn more
- The Food and Research Action Center’s website has extensive information on school lunch and breakfast programs, including program impacts, eligibility requirements, and reimbursement.
- The Cost of School Lunch, produced by School Food Focus, provides a breakdown of school lunch costs.
- The Food and Research Action Center ‘s School Meals Legislation and Funding by State provides information on state mandates regarding school breakfast and lunch and state funding to support the programs.
- The Healthy Schools Campaign and Trust for America’s Health co-convene the National Collaborative on Education and Health to increase cross-sector collaboration to improve health and education outcomes. Focus areas include health and wellness metrics, health system transformation, chronic absenteeism, substance misuse, and mental health.
- The USDA Economic Research Service report, Children’s Food Security and USDA Child Nutrition Programs, examines food insecurity rates and the effectiveness of the school meal and other child nutrition programs on alleviating food insecurity.
- The School Nutrition Association offers extensive resources and research on all aspects of school meal programs, including administration, marketing, nutrition, and pertinent legislation.
- The Alliance for a Healthier Generation offers multiple resources focused on creating healthier school environments, including the Healthy Schools Program Framework of Best Practices.
